Urgent Conversations Around Breast Cancer and Black Women – Raising Awareness & Bridging Gaps
Lifestyle
|
Oct 30, 2023
|
5 MIN READ
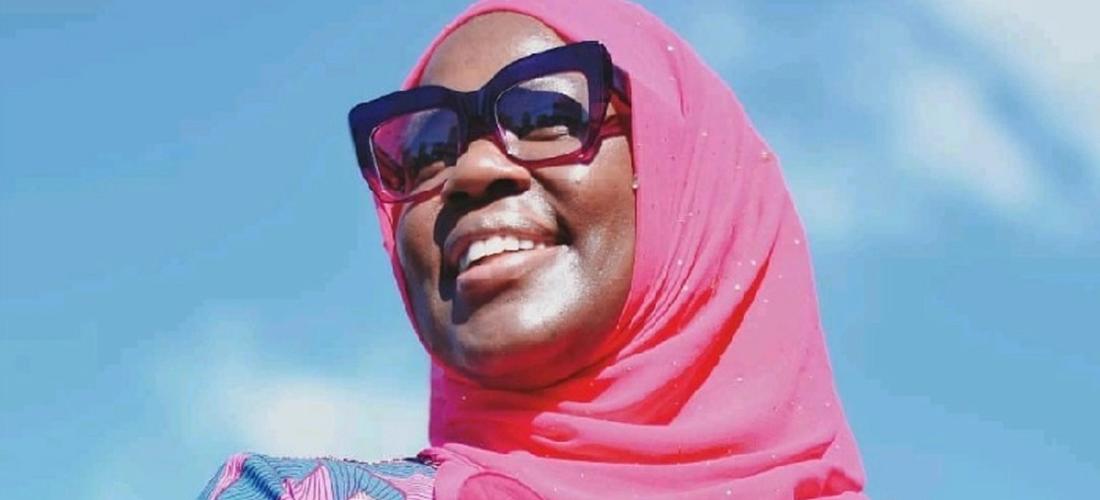
Dr. Ramla N. Kasozi, Mayo Clinic College of Medicine and Sciences; image source: LinkedIn
As Breast Cancer Awareness Month comes to a close, it's essential to understand that breast cancer is not a one-size-fits-all illness. The disease disproportionately affects Black women with higher mortality rates than white women, highlighting the need for targeted awareness and specific interventions for this community.
According to the American Cancer Society, Black women are about 40 percent more likely to die from breast cancer than white women, even though they have a 4 percent lower incidence rate. So, while Black women may be less likely to get breast cancer, they are more likely to die from it.
I asked Dr. Ramla Namisango Kasozi to share her insights about Black women and breast cancer and offer some advice. Dr. Ramla is a board-certified family medicine physician and public health specialist. She is a Senior Associate Consultant in the Department of Family Medicine and Assistant Professor of Family Medicine at Mayo Clinic College of Medicine and Sciences.
Risk Factors as it Pertains to Black Women
Breast cancer is a devastating, indiscriminate disease afflicting women of all different backgrounds. Women of any age can be affected, and the disease is unfortunately all too common. “All women are at risk of breast cancer,” Dr. Ramla explains, “However, Black women die earlier from breast cancer at a median age of 62 compared to White women at 69 years [of age].” The higher breast cancer death rate for Black women demonstrates a significant and troubling health disparity that needs immediate attention.

Dr. Ramla N. Kasozi
This elevated mortality rate is not just a statistic; it represents countless lives, families and communities who are disproportionately impacted. The disparity is a complex issue with multiple layers, including but not limited to biological factors, systemic inequalities and cultural stigmas.
Dr. Ramla shared some factors that may contribute to the mortality disparity, which include but aren’t limited to:
- Barriers to early screening and detection.
- Delay in seeking care.
- Lack of insurance.
- Fear of testing.
- More advanced stages of disease at diagnosis among minorities,
- Unequal access to chemotherapy once a breast cancer diagnosis is made.
Other common factors that may contribute to these disparities (these are factors one can’t change themselves) include:
- Having genetic mutations (inheriting mutations BRAC1 and BRCA2).
- Reproductive history: menses before age 12 and menopause after 55 expose women to hormones longer.
- Having dense breasts (hard to see tumors on a mammogram).
- Personal history of breast cancer or certain non-cancerous breast diseases.
- Family history of breast or ovarian cancer.
And finally, other risk factors )that are modifiable) include:
- Not being physically active (due to limited access to green spaces to walk/run, limited access to the gyms and sporting places).
- Being overweight or having obesity after menopause.
- First pregnancy after age 30, not breastfeeding.
- Drinking alcohol
- Smoking

Image source: Pexels
Dr. Ramla stresses access to healthcare as a significant risk factor. “Black women face unique challenges with having access to the healthcare system and primary care services,” she said. “This includes going to preventative appointments to have biennial mammograms. Some studies suggest that Black women do not receive adequate treatment compared to their counterparts despite improvements in early detection and screening.
“To mitigate this, efforts are being made to focus on preventative health by offering education about breast cancer screening at every healthcare visit.” she says.
The Importance of Regular Mammograms
Mammograms play a crucial role in breast health by providing an early detection method for breast cancer. This diagnostic tool uses low-dose X-rays to create images of breast tissue, allowing healthcare providers to identify abnormalities or changes over time. Early detection significantly improves the chances of successful treatment and can lower mortality risk. Dr. Ramla encourages women to get scheduled mammograms.
“I recommend all women, especially Black women, consider having a mammogram starting at age 40. I always try to discuss breast health and the importance of mammograms every 1-2 years.
“Always ask your healthcare provider if you are due for a mammogram at every visit. If not, encourage your healthcare provider to schedule it in advance so that you can mark it in your calendar to do the imaging. Most healthcare institutions allow women to schedule mammograms without a doctor’s visit,” she says. "Fortunately, there are various mobile mammogram units in different cities in the U.S., so Black women must empower themselves to research such as outreach activities in their respective communities.”
Getting your breasts squished every couple of years is a small price to maintain their health and increase the potential of early detection if something is wrong
(Not sure what a mammogram entails? Our Blog Editor Dilshad takes you through the entire process.)
Receiving news of an abnormal mammogram can be an emotionally overwhelming experience filled with anxiety and uncertainty. The term "abnormal" can trigger an immediate fear of a cancer diagnosis, although it's crucial to remember that not all abnormalities are cancerous. The emotional toll can be particularly intense for Black women, who are aware of the higher mortality rates and more aggressive forms of breast cancer that disproportionately affect their community.

Image source: Pexels
Dr. Ramla encourages Black women to pay attention to their breasts and expect support from their healthcare providers. “Black women must continue to advocate for their breast health and speak with their primary care provider about access to biopsies if one has an abnormal mammogram and effective treatment if breast cancer is diagnosed,” she says. “Furthermore, healthcare providers are expected to act quickly once an abnormal mammography is sent to them.”
Urgent Need for Multidimensional Interventions
Addressing the higher breast cancer death rate among Black women requires a multifaceted approach that includes:
1. Policy changes: These can make preventative care and treatment more accessible and affordable.
2. Culturally competent medical care: Physicians and healthcare providers must be trained to understand and address the specific challenges and barriers Black women may face.
3. Community education: Targeted awareness campaigns are necessary to educate Black women about the importance of early screening and detection.
4. Research: More research funding to investigate why Black women are more susceptible to aggressive forms of breast cancer and to develop effective treatments for these types.
By collectively addressing these aspects, we can reduce the high breast cancer mortality rate among Black women and move toward a more equitable healthcare system. The higher death rate is not just a medical issue; it's a social justice issue that calls for immediate and comprehensive action.
Breast cancer is not a singular experience; it is intersectional, affecting each woman differently based on various factors, including race and ethnicity. Let’s use this month, and every month, to address these disparities head-on.
Subscribe to be the first to know about new product releases, styling ideas and more.
What products are you interested in?


